Abdominoplasty – Tummy Tucks Complications and Risks
So you think of abdominoplasty (tummy tucks) what are the possible complications of Abdominoplasty (tummy tucks)?? Are they easily avoided I’m not telling you these complications to make you afraid of abdominoplasty (tummy tucks) but because technically I always prefer the patient be aware of his surgery complications and steps.
Here is the list of possible complications of Abdominoplasty (tummy tucks)
Anesthesia reaction:
This is reaction during surgery because of anesthesia
Belly button death:
More Common in Smokers Occurs Due to failure of healing of 2 surgical scars
Bleeding
Hematoma (risk is 3-4%)
Collections of blood
Infection (risk is less than 1 %)
Not common as surgeries are done in septic conditions
Keloid:
Heavy scar
Puckered skin
Skin Lesions in which skin is wrinkled
Reactions to medications
Seroma
Skin irregularities
Skin necrosis or skin death (more likely with smokers)
Slow healing
Suture Rupture
Swelling
Visible scar
Serious complications after an abdominoplasty are uncommon. However, there are risks with any surgery and specific complications associated with this procedure.
Complications such as infection and blood clots are rare, but can occur. Infection can be treated with drainage and antibiotics, but will prolong your recovery. You can minimize the risk of blood clots by moving around as soon after the surgery as possible (immobility allows blood to pool and create a clot which can travel to the lungs, heart or brain causing a pulmonary embolism, heart attack or stroke).
If wound problems develop, it may delay healing for several weeks or even months. Areas of skin may die and slough off (this complication is more common among smokers). This will result in delayed healing and may require a skin graft. Although rare, it is possible for fat to liquefy and drain through the incision. Additional surgery may also be necessary.
One of the more common problems after an abdominoplasty is collection of fluid under the skin after the drains have been removed. Your surgeon can aspirate the fluid with a needle. The drainage stops within a month and will not affect the final results.
Scars
Surgical scars -as complication of Abdominoplasty (tummy tucks) – are permanent. There will be a long scar extending from hip to hip. However, the incisions are usually placed below the swimsuit line so they will not normally be in view. Your scars may actually worsen during the first three to six months as it heals, but this is normal. It normally takes 9 months to a year before scars flatten out and lighten in color.
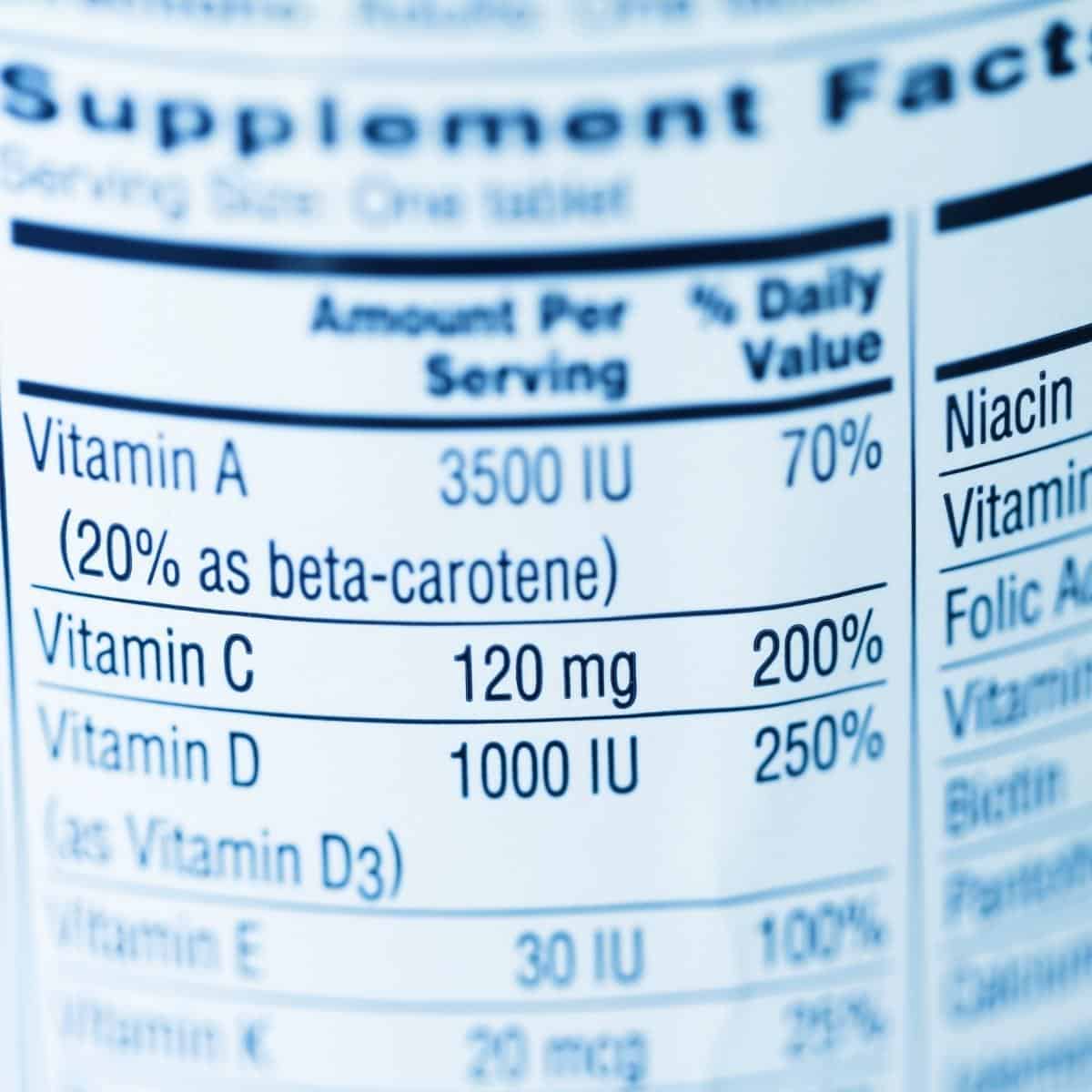
Nutritional Consequences
Protein Deficiency complication
Abdominoplasty (tummy tucks) is a metabolic surgery designed to produce malnutrition. Energy deficit occurs due to low food intake, food intolerance, and nutrient malabsorption. Abdominoplasty (tummy tucks) aim to achieve malnutrition to lose weight but without complications.
Protein deficiency can occur after Abdominoplasty (tummy tucks).The ratio of fat mass to fat-free mass loss is about 4:1 unrestrictive operations like RYGB.12 It is probably even more severe after biliopancreatic diversion (BPD). The literature isn’t clear. Some report severe protein-calorie malnutrition13although low incidences have been described by others.
Protein deficiencies manifest themselves initially with fatigue and loss of muscle strength, especially with greater than expected weight loss as in patients who have strictures of the gastrojejunal anastomosis. Progression of protein deficiency is predictable with continuing weight loss with the additional development of hair loss, poor wound healing, wasting, emaciation, kwashiorkor, and marasmus.
Protein deficiencies should be addressed promptly with supplementation. Although normal protein requirement for the average individual is 1 g/kg body wt/day, this formula does not work for the morbidly obese with weights of 200 kg more. Most Abdominoplasty (tummy tucks) surgeons aim for 60-90 g per day for their postoperative -Abdominoplasty (tummy tucks) -patients, but, in fact, there is little evidence for this guideline. Protein deficiency can be assessed by checking serum albumin levels at regular intervals, but it isn’t a reliable measure. We have seen virtual normal albumin levels in patients who were severely malnourished that fall to extremely low values when additional nutrition is provided. It almost appears that the patients lack the enzymes to utilize the albumen, building albumen stores that cannot be used.
Approach is to proceed promptly by supplementing these patients with one or two cans of a liquid, high protein, high vitamin preparation such as Ensure Plus if they are able to tolerate an oral diet. This approach rarely fails but may take weeks to restore patients to euproteinemia.If the patients are unable to eat or drink, however, total parenteral nutrition should be started promptly with an emphasis on slow rather than fast correction. In our experience, badly malnourished patients should be corrected slowly; they are unable to manage sudden large loads of nutrients when they are first seen.
Carbohydrate Deficiency Complication
Carbohydrate deficiency, manifested as episodic hypoglycemia, is probably quite common. Many patients admit to having episodes of feeling “shaky and light-headed” during the day, usually about 2 hours or so after meals. When our series of gastric bypasses was about 1000 cases over 16 years, we found 47 patients in our practice who developed documented glucose levels in the 30-40 d/mL range. The hypoglycemia appeared to be independent of age, gender, race, original weight, and degree of weight loss and could appear as late as 14 years after the operation. Fortunately, all of our patients were managed well with candy taken at the first “aura” of hypoglycemia, i.e., weakness, shaking, sweatiness, etc. All cleared within a year of the appearance of symptoms. A recent report of nesidoblastosis requiring pancreatic resection suggests that refractory cases exist possibly due to the development of secondary tumors.